Dirofilaria repens is one of 40 species of Dirofilaria. It is a zoonotic filarial nematode that commonly impacts dogs, however, human infection can occur through affected organs like skin, lung and eyes [1]. Although, there have been case reports of Dirofilaria on the Indian subcontinent [3,4], studies highlight it to be an endemic in the Mediterranean peninsula [1,2,5,6].
Within the last few years, due to the increasing tourism and immigration, there is increasing evidence of the disease being presented in various parts of the world [1-6]. Previous case reports have already isolated the worm from various ocular regions, from the subconjunctiva or Tenon’s layer, perioribital tissues to the anterior chamber and the vitreous [3]. Patients can present with a vast number of symptoms; however, a common complaint from patients is the ‘sensation of a foreign body moving in or near their eye’ and itchiness, with concomitant swelling and conjunctival redness [1,2,6].
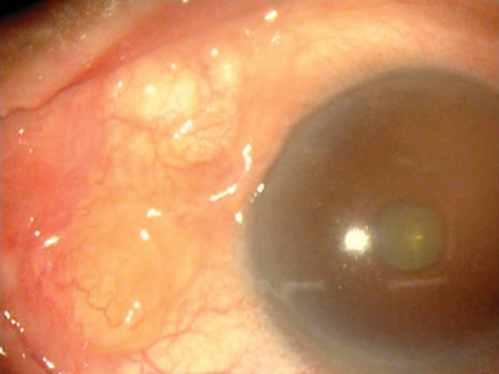
Figure 1: Highlighting the Dirofilaria worm in the anterior chamber.
Case report
A 65-year-old Sri Lankan gentleman who has been living in the UK for the last 35 years presented to the eye casualty with a three-week history of a red eye. The patient was seen by his GP and treated as conjunctivitis. The patient’s symptoms persisted and a further review in eye casualty led to the diagnosis of episcleritis and a treatment dose of steroids was prescribed and the patient was discharged. The patient is known to travel back and forth to Sri Lanka.
Despite the treatment, the patient’s symptoms deteriorated. It was noted by his son, who is a GP, that there was a moving foreign body in his sclera. He was promptly taken to the eye casualty. The moving foreign body was identified as nematode and a plan to surgically remove it in clinic was made. With the worm freely moving under the microscopic light, the ophthalmologist applied subconjunctival lignocaine which subsequently paralysed the worm. A sub-conjunctival incision was made and the worm was removed. The worm was placed in a microbiological bottle and the specimen was sent to the London school of tropical medicine. It was later identified as Dirofilaria repens.
Discussion
This case report along with the others highlights an increasing incidence of Dirofilaria repens around the world with seldom few case reports being noted in the UK [6]. Seventy percent of all documented cases were from 2006-2012 [2]. It is important to stress this infection as an environmental hazard in certain climates due to its zoonotic transmittance from dogs and mosquitoes [5]. Recent patient travel can be vital in the diagnosis as after inoculation adult worms can take two weeks to reach the infective stage and can survive for several years in the human [2,6]. The microfilaria creates a subcutaneous home where it matures [6]. Other than patient history, an infection with Dirofilaria repens is diagnosed histopathogically upon surgical excision [2]. Dirofilaria can impact a variety of other organs; ranging from pulmonary, subcutaneous [5], cerebrum, testicles and female breast [2]. Subretinal infiltration of this nematode can lead to severe uveitis and ultimately blindness as it moves into the subretinal space [2]. Ophthalmologists can potentially be the first source of detection of Dirofilaria repens and it is important that surgical extraction and an expedited referral to a tropical disease hospital occur. Removal of the worm is carried out under local anaesthetic with forceps. The Dirofilaria repens does not require systemic treatment, unlike cases of ocular Loa Loa [1,4].
References
1. Khoramnia R, Wegner A. Subconjuncitval Dirofilaria repens. The New England Journal of Medicine 2010;363:e37.
2. Kalogeropoilos CD, Stefaniotou MI, Gorgoli KE, et al. Ocular Dirofilariasis: A case series of 8 patients. Middle East African Journal of Ophthalmology 2014;21(4):312-316.
3. Bhat KS, Kotigadde S, Vishwanatha BK, Pare P. Subconjunctival dirofilariasis: Case studies with review of literature. Tropical parasitology 2014;4(2):119-21.
4. Bowler GS, Shah AN, Bye LA, Saldana M. Ocular loiasis in London 2008-2009: a case series. Eye 2011;25:389-91.
5. Senanayake MP, Infaq ML, Adikaram SG, Udagama PV. Ocular and subcutaneous dirofilariasis in Sri Lanka infant: an environmental hazard caused by dogs and mosquitos. Paediatric International Child Health 2013;33(2):111-2.
6. Knapman AJ, Booth AJ, Farnworth D. Return of the cosmopolitan worm. Eye 2003;17:791-3.
COMMENTS ARE WELCOME