As ever, I would like to thank all those who participated in the last edition’s survey. A lot of data was generated and I do not intend to go through each individual finding. What is staggering again is the degree of variability we see in what clinicians consent for and in their views as to what is important or not.
I have previously mentioned that the Bolam Test for clinical negligence no longer applies to consent. Previously, if our consent process was supported by a reasonable body of professional opinion then we would not be negligent. Montgomery changed all that and rightly so, to some degree. We have a very unique speciality with concepts that are hard to understand. I remember when I began my eye training. I had been on the general surgery rotation and had obtained my MRCS before swapping to ophthalmology. Despite being medically and surgically trained, and those two pitifully short weeks in ophthalmology as a medical student, I had no idea what the posterior capsule was all about or what swelling in the retina could do. How can we then expect patients to get a grip on these quite complex and nuanced issues?
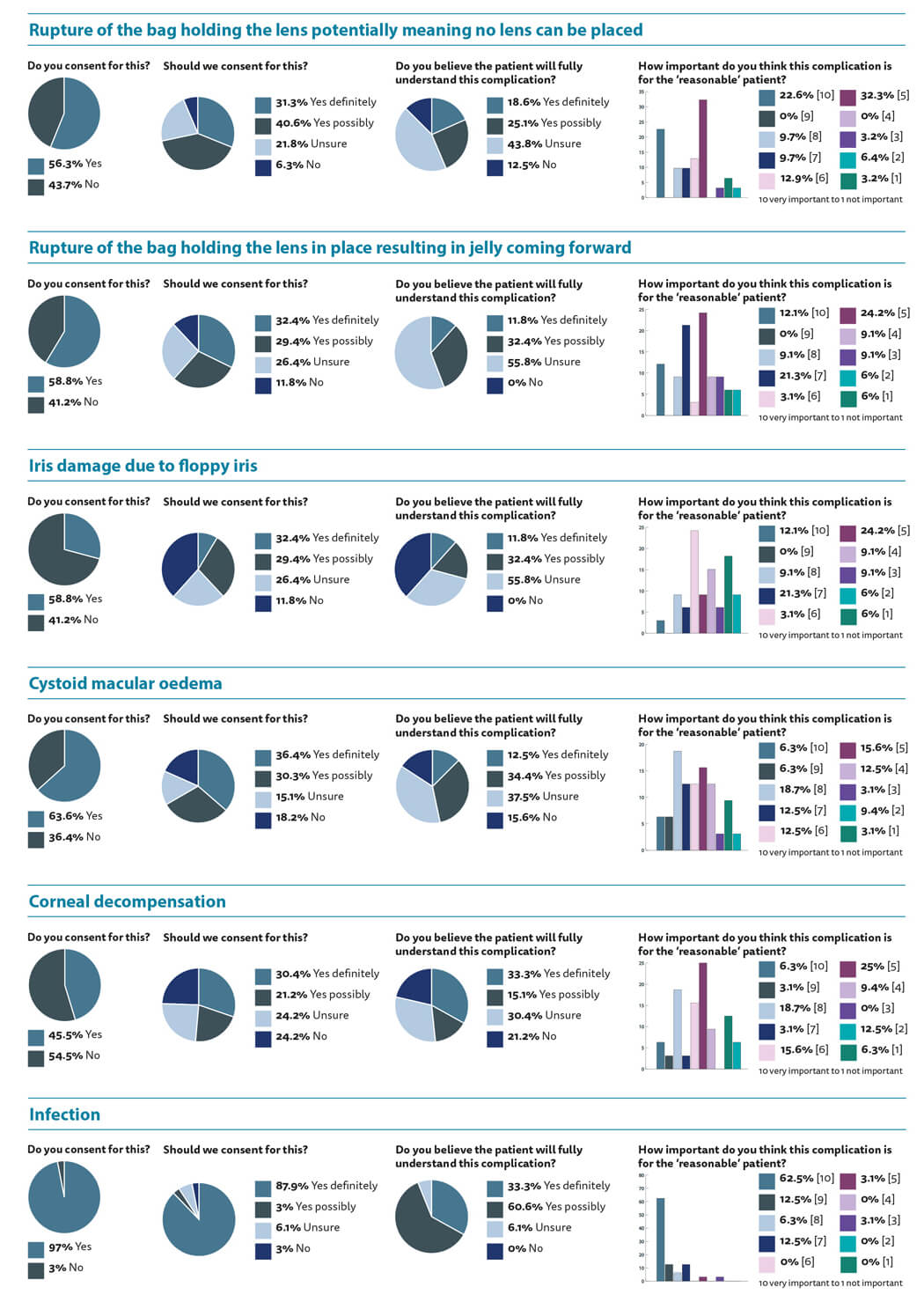
We need to look at the reasonable patient and what material risks they need to know and yet the survey outcomes clearly show that as a profession we do not really agree on what should or should not be told to the ‘reasonable’ patient. How can medical experts advise the courts as to what is a breach of duty, if we cannot agree amongst ourselves and some opinions are very polarised?
It seems that we are all in agreement that the risk of irreversible visual loss and the chance of the lens falling to the back of the eye should be discussed with the patient. As should the need for spectacle correction postoperatively, although this is clearly not a complication per se, but there is a 50:50 split regarding the need to consent regarding the need for laser treatment which, again, I would not consider a complication. It begs the question as to what should be in a patient information leaflet and what should be on the consent form?
I will leave the reader to assess the outcomes from the pie charts. What is striking is the variance within the bar charts. Some clinicians feel that a certain complication is not important at all, while others rate it a 10, indicating high importance. I would also like to draw the readers’ attention to the outcomes to the question regarding the patient’s understanding. Should we be consenting patients for a complication we do not believe they will genuinely understand?
The last few questions show that the majority of us use pre-printed consent forms. I agree with the majority that the consent process should be around five minutes and I am envious of those clinicians who have more than 20 minutes to spend solely on the consent part of the cataract consultation. No wonder they have time to discuss every complication under the sun.
Eighty-five percent of us believe that patients would not wish to know every risk, which fits with the need to tell the patients about ‘material’ risks. Forty-one percent of us feel that if a patient does not want to know all the risks we should respect that. Is that not the fundamental principal of respecting a patient’s wishes? Should we force patients to listen to risks they do not want to hear? I will leave it to the readership to consider whether we still get the patient to sign the consent form even though we have not detailed the risks contained therein.
Finally, there seems to be a bit of uncertainty regarding complications not on the consent form. Whether a complication is on the consent form or not, if the clinician breached duty and behaves negligently then they are liable. Even if posterior capsule rupture (PCR) is on the consent form and the patient loses vision because it occurs, it does not protect us from litigation. If the PCR occurred due to negligence then the patient can still claim for compensation. Equally, if a patient encounters a complication which was rare and unforeseen then it does not necessarily breach the duty of care regarding consent if it were not on the consent form. Does it matter how exactly the complication occurs or is it more important to the patient to consider the likelihood of visual loss, which may or may not be remediable?


COMMENTS ARE WELCOME






