Once more I would like to thank those of you who took the time to complete the last edition’s survey. It was highly pertinent to what we are facing now.
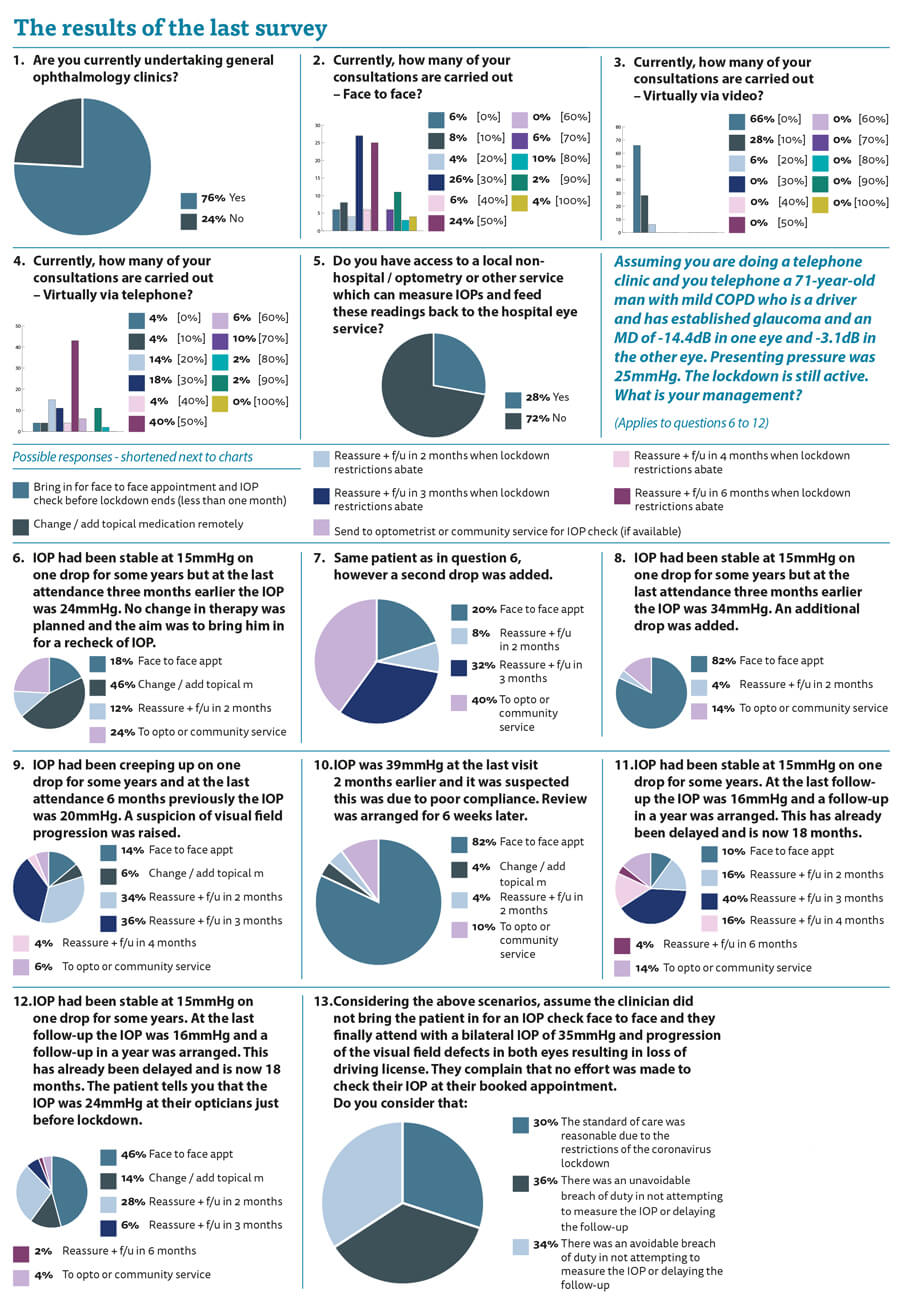
It is clear that our services have been markedly disrupted. Three quarters of us are seeing 50% or less of our patients face to face in clinics, with a lot of us telephoning patients for their consultations. I have done my fair share of trying to guess the intraocular pressure (IOP) from the timbre of the patient’s voice over the phone and the jury will remain out for some time as to whether I am getting it correct.
Only one quarter of us have access to some other mechanism to check patients IOPs which I think is concerning.
The clinical scenario I presented to you is common. A patient who was stable and ‘low risk’ on one drop who was due for a clinical review to check them has been hamstrung by the lockdown.
When faced with our hypothetical stable patient we assessed the clinical record and found that their IOP was 24mmHg at their last attendance and they were due for a recheck which was cancelled by COVID-19 issues. Almost half of responders would have given topical medication remotely without seeing the patient again. A quarter would have organised a face to face (F2F) appointment within two months and a quarter would have asked the patient to attend an optometry or community service for an IOP check. My personal view is that all of these options are entirely reasonable.
When a second drop was added at the last visit, we need to check efficacy. We know there is a non-response rate, however, on the balance of probabilities, we can reasonably assume that there was some response and the IOP should have come down. Even if there was not a massive response an IOP of 24mmHg is unlikely to cause a rapid deterioration. Forty percent would be happy with a community IOP check, while one-fifth would bring the patient in within a month for a F2F appointment.
Now the IOP is higher at 34mmHg and there are clear clinical risks if the IOP does not respond. In this scenario the majority would bring the patient in for a F2F review. But this is not universal and there are some clinicians who would still bring patients back in two months. If at that time the IOP was 40mmHg would they be protected as having acted reasonably?
When the IOP was still not particularly high but there was a suspicion of visual field progression, the majority of clinicians would arrange an appointment for two to three months. I think this is reasonable as glaucoma progresses slowly and the IOP was not particularly high.
When faced with an IOP of 39mmHg and suspected poor compliance the majority would have brought the patient in for a review within one month. Some would add a drop remotely but if they are already non-compliant it seems strange to expect them to use an extra drop.
When we are considering a patient who has been stable and has already had their appointment delayed, the view on what we should do starts to broaden. We planned to see this patient at a year. They have already been delayed, which we know is a problem and is causing visual loss. The patient remains low risk but not no risk. If their IOP had gone up gradually then they could be sitting with an IOP of 32mmHg for more than a year now. Approximately a quarter would prioritise this patient and bring them in in one or two months. More than half would bring the patient back in three to four months, meaning their final F2F and IOP check is potentially almost a year delayed.
In the next scenario we know that the IOP has gone up as it was checked by the optician. This changes practice and now the follow-up is much tighter. The only difference between this case and the one above is that they happened to go to their optometrist for an eye check before lockdown and they measured the pressure as being high. Is it better not to know the true pressure, as in the previous case? Does that mean that these two cases deserve different management because we do not know what the pressure is?
The final question deserves reiterating. “Considering the above scenarios, assume the clinician did not bring the patient in for an IOP check face to face and they finally attend with a bilateral IOP of 35mmHg and progression of the visual field defects in both eyes resulting in loss of driving license. They complain that no effort was made to check their IOP at their booked appointment.” How should we as a professional body respond? How should the expert witnesses and the Courts interpret the situation? Does the coronavirus crisis give us enough leeway to protect ourselves from these undesirable decisions we are making?
Thirty percent of respondents felt that the standard of care was reasonable due to the restrictions of the coronavirus lockdown. Thirty-six percent of responders felt that there was unavoidable breach of duty in not attempting to measure the IOP or delaying the follow-up.
So, two thirds of the respondents would excuse the decisions based on the fundamental and unprecedented pressures we have faced due to the coronavirus and I would be sympathetic with that, but would the Courts?
A third felt there was an avoidable breach of duty in not attempting to measure the IOP or delaying the follow-up. If one third of our respondents felt that then what should the Courts believe, and will we be criticised when judgment day comes?
I hope that this stimulates thought and debate about the standard of care we are providing and we ensure that we are doing our best for the patients. As ever, some guidance from those much wiser than me would be welcome.
COMMENTS ARE WELCOME






