Sands of Sahara syndrome (diffuse lamellar keratitis) is a rare postoperative complication of Laser in situ keratomileusis (LASIK). Its estimated prevalence is reported to be 2-4% among LASIK cases [1], despite that, it is more likely to be encountered by the eye casualty doctor due to the increasing numbers of patients undergoing LASIK surgery every year.
In this report we provide a systematic approach to the diagnosis of this condition using slit-lamp examination and anterior segment imaging modalities, as well as a simplified regime for treatment and follow-up.
In LASIK surgery a corneal flap is created using either a microkeratome or femtosecond laser, the stromal bed is then ablated using excimer laser and the flap is repositioned [2]. Diffuse lamellar keratitis (DKL) is characterised by inflammatory infiltration beneath the flap leading to granular whitish corneal deposits, hence the name ‘Sands of Sahara’ [3].
The characteristic clinical presentation in DLK develops one to two days following refractive surgery and typically resolves five to eight days after the initiation of appropriate therapy [4]. The post-surgical corneal opacification that accompanies DLK is typically sterile and sub-epithelial [3].
Pathogenesis of DLK remains controversial, the current theories indicate that manipulation of corneal surface during surgery initiates the inflammatory reaction, also having an epithelial defect increases the chances of DLK by 24 times [5]. Intraoperative factors attributed to the pathogenesis of DLK include blood cells, fine sponge fibres or meibomian gland secretions present at the flap-stromal interface [6]. A documented case series of DLK found that toxicity from the marking pen could result in DLK [7].
Case presentation
A 36-year old female presented to the eye casualty at the Great Western Hospital in Swindon with a one-day history of red painful eyes, blurred vision and sensitivity to light. The condition was of sudden onset and the patient denied trauma or contact lens use. There was no past medical history of significance, she gave a history of bilateral LASIK surgery 15 months prior to presentation. The patient doesn’t drive and is not known to be allergic to any medications. Visual acuity (LogMAR) was 0.04 in the right eye and 0.10 in the left, the right eye showed marked degree of diffuse conjunctival injection as well as localised limbal injection (Figure 1).

Figure 1: Marked degree of diffuse conjunctival injection as well as circum-limbal injection (arrows).
There were multiple white granular deposits in the flap-corneal interface. There was no epithelial defect and the intraocular pressure was normal (Figure 2).

Figure 2: Multiple white granular deposits in the flap-corneal interface.
Anterior segment OCT showed diffuse hyper-reflective dots in the flap-stromal interface (Figure 3). A clinical diagnosis of diffuse lamellar keratitis was made.
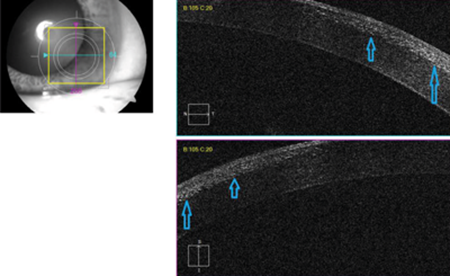
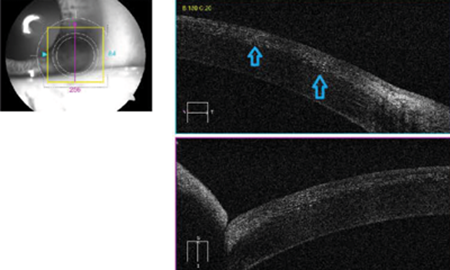
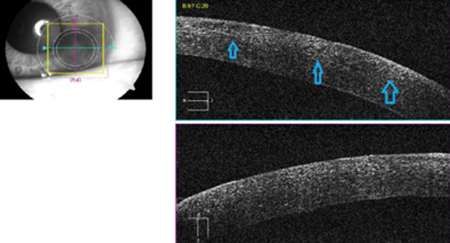
Figure 3: Anterior segment OCT showed diffuse hyper-reflective dots in the flap-stromal interface.
The patient was started on Dexamethasone 0.1% preservative-free eye drops four times daily, together with Chloramphenicol 0.5% preservative-free eye drops four times daily, both to the right eye. Five days later, there was complete resolution of symptoms and the cornea clarity was restored on examination.
Discussion
We aim to provide a systematic approach that facilitates recognising and managing this relatively rare condition. Our case is atypical in its late presentation which is not known about DLK. The initial step is to obtain detailed history including the onset and progression, the important negatives like contact lens wearing and the past ophthalmic history. It would be ideal to have a copy of the operation note to look for any documented intraoperative complications. This is followed by slit-lamp corneal examination using a narrow bright beam of light at 60 degrees angle and high magnification looking for any interface pathology. Anterior segment OCT is of great help in identifying the character and depth of deposits and serves as a method of both documenting and monitoring the progress.
The clinical features of DLK are as follows:
Stage 1: Peripheral corneal infiltrates without central involvement.
Stage 2: Migration of inflammatory cells into the central cornea with visual impairment.
Stage 3: Corneal scarring.
Stage 4: Stromal melting.
Standard treatment is to start topical preservative-free steroid eye drops with broad spectrum antibiotic cover and close monitoring. Other methods of management include surgical lifting of the flap and wash out of the interface. DLK usually carries a good prognosis, response to topical treatment alone is usually quick provided that there are no other co-pathologies.
Conclusion
DLK represents a diagnostic and therapeutic challenge. Such cases are expected to become more common in the coming years as LASIK is becoming more widely available and affordable. Lack of clinical expertise in this field adds to the challenge and hence the need for a standardised and systematic approach like this one.
References
1. Azar DT, Koch DD. LASIK: Fundamentals, Surgical Techniques and Complications. New York: Marcel Dekker Inc; 2003.
2. Kanski JJ, Bowling B. Clinical Ophthalmology A Systematic Approach. Philadelphia: Saunders; 2011.
3. Smith RJ, Maloney RK. Diffuse lamellar keratitis. A new syndrome in lamellar refractive surgery. Ophthalmology 1998;105(9):1721-6.
4. Messmer JJ. LASIK: a primer for family physicians. Am Fam Physician 2010;81(1):42-7.
5. Shah MN, Misra M, Wihelmus KR, Koch DD. Diffuse lamellar keratitis associated with epithelial defects after laser in situ keratomileusis. J Cataract Refract Surg 2000;26(9):1312-8.
6. Davis EA, Fahmy AM. Stage III diffuse lamellar keratitis following conductive keratoplasty over a LASIK flap. J Cataract Refract Surg 2009;35(6):1141-3.
7. Hadden OB, McGhee CN, Morris AT, et al. Outbreak of diffuse lamellar keratitis caused by marking-pen toxicity. J Cataract Refract Surg 2008;34(7):1121-4.
COMMENTS ARE WELCOME





