Angioid streaks (AS) may be associated with pseudoxanthoma elasticum (PXE), Paget’s disease, haemoglobulinopathies, Ehlers-Danlos Syndrome or abetalipoproteinaemia. Histopathology showed retinal pigment epithelium (RPE) and choriocapillaris loss, elastic fibre degeneration, calcium deposition, active choroidal neovascular membrane (CNVM) and vascular endothelial growth factor (VEGF) accumulation within Bruch’s membrane, and increase in vascular endothelial cells and fibroblasts [1].
Matrix metalloproteinase-9 (MMP-9) and hypoxia inducible factor (HIF-2α) influence AS pathogenesis [2]. This report highlights the effect of apparently trivial trauma on the eye of a patient with AS and subtle signs of PXE.
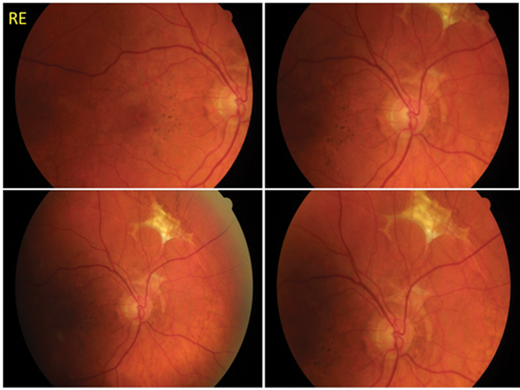
Figure 1a and b: Angioid streaks (AS) in a 46-year-old gentleman who presented 10 days following minor trauma to his LE with reduced vision. Funduscopy of (a) RE revealed crack-like dehiscences with peripheral scar tissue in superonasal retina and (b) LE showed foveal choroidal neovascular membrane with scarring and multiple choroidal ruptures that developed despite treatment with intravitreal injection of anti-VEGF bevacizumab (Avastin). Diagnosis of PXE was confirmed by skin biopsy.
Case report
A 46-year-old male presented to the eye casualty 10 days after accidental trauma involving a tree branch hitting his left eye. Four days later he developed a black eye and blurring of central vision. Visual acuity was 0.04 RE and 0.98 improving to 0.64 LE. Fundus examination revealed bilateral peripapillary AS with peripheral scar tissue in RE (Figure 1a) and multiple choroidal ruptures with intraretinal haemorrhages in LE (Figure 1b). The diagnosis appeared to be that of PXE associated AS.
Optical coherence tomography (OCT) of LE showed evidence of CNVM. Fundus fluorescein angiography (FFA) showed multiple choroidal ruptures and CNVM with leakage. He was treated with a stat intravitreal anti-VEGF injection (1.25mg Avastin). However, organisation and fibrosis of the left macula produced a disciform scar and vision eventually reduced to hand movements.
Dermatology review confirmed PXE in the presence of mild skin involvement (yellowish appearance of dimpled skin over the lateral aspect of both axillae) and positive skin biopsy.
Comment
The diagnosis of AS was incidental at his delayed presentation post minor trauma. Associated features of AS including pattern dystrophy, drusen of the optic nerve, peripheral ‘comet tail’ lesions and autofluorescent perimacular white spots were not seen [3]. Dermatology review revealed an absence of abnormal skin around his neck or other flexures and a negative family history of PXE.
PXE is a connective tissue disorder (mutation in ABCC6 gene, Chr16p13.1) with features of calcification and fragmentation of elastic fibres in the dermis, eye and cardiovascular system. ABCC6 gene codes for multidrug resistance-associated protein 6 (MRP6) [4]. Reduced MRP6 alters blood levels of uncharacterised metabolites causing ectopic mineralisation and x-ray analysis shows elevated glycosaminoglycans [5]. The pull of intrinsic and extrinsic ocular muscles on the optic nerve creates lines of force causing RPE dimpling (peau d’orange) and later breaks with similar configuration to peri-papillary interlacement and radial extensions [6].
Complications of AS include CNVM and sub-retinal haemorrhage caused by traumatic choroidal rupture. A case of polypoidal choroidal vasculopathy, proposed to represent a variant of CNVM has also been reported [7]. Treatment options include:
- Observation: Amsler grid and FFA in symptomatic patients characterised by early hypofluorescence in the A-V phase and late hyperfluorescence reveals progressive central vision loss.
- Laser photocoagulation: Improved outcomes for lesions located at least 100um from foveal centre, however higher recurrence (77%) noted compared to other conditions (age-related macular degeneration [AMD], degenerative myopia and histoplasmosis).
- Surgical: Removal of CNVM without significant damage to RPE and neurosensory retina. Poor outcomes are described in older cases with subfoveal bleed, atrophic RPE and recurrent CNVM [8].
- Photodynamic therapy (PDT): For cases with classic subfoveal CNV with short-term reduced size of leakage.
- Intravitreal anti-VEGF: Successful outcomes following a) Avastin 1.5mg (up to x3 injections) [9] or b) monthly intravitreal injections of 0.5mg Lucentis with average improvement from baseline best corrected visual acuity (BCVA) of 6/18 to 6/9 after 12 months maintained up to three months post treatment have been described [10].
Conclusion
- This incidental diagnosis of AS highlights the importance of fundus examination in all ocular trauma cases.
- OCT is an easily available and vital tool in diagnosis and charting prognosis.
- FFA is helpful in confirming the diagnosis and identifying complications.
- Multidisciplinary approach, dermatology review in this case.
- Poor visual prognosis, with recurrent CNVM causing moderate to severe vision loss in 70-86%.
- Advantages of intravitreal anti-VEGF including Avastin or monthly Lucentis IVI.
Acknowledgements
Mrs Chitra Madhavan, Consultant Ophthalmologist in Medical Retina; Mrs Angie Smith, Senior Orthoptist for her excellent fundus imaging and, of course, the patient (TR) without whom this case report would not have been possible.
References
1. Jensen OA. Bruch’s membrane in pseudoxanthoma elasticum. Histochemical, ultrastructural, and x-ray microanalytical study of the membrane and angioid streak areas. Graefes Arch Klin Exp Ophthalmol 1977;203:311-20.
2. Kazato Y, Shimida H, Nakashizuka H, et al. Immunohistochemical findings of a Bruch’s membrane defect and active choroidal neovascularization in angioid streaks. Jpn J Ophthalmol 2010;54:172-4.
3. Trelohan A, Martin L, Milea D, et al. Retinal lesions in PXE: 51 patients. French Journal of Ophthalmology 2011;34(7);456-67.
4. Hesse RJ, Groetsch J, Burshell A. Pseudoexanthoma elasticum: a novel mutation in the ABCC6 gene that affects eye manifestations of the disease. The Ochsner J 2010;10(1):13-5.
5. Klement JF, Matsuzaki Y, Jiang Q-J, et al. Targeted ablation of the ABCC6 gene results in ectopic mineralization of connective tissues. Mol Cell Biol 2005;25:8299-310.
6. Li Q, Sadowski S, Uitto J. Angioid streaks in pseudoxanthoma elasticum: role of the p.R1268Q mutation in the ABCC6 gene. J Investig Dermatol 2011;131(3):782-5.
7. Baillif-Gostoli S, Quaranta-El MM, Mauget-Faysse M. Polypoidal choroidal vasculopathy in a patient with angioid streaks secondary to pseudoxanthoma elasticum. Graefes Arch Clin Exp Ophthalmol 2010;248(12):1845-8.
8. Eckstein M, Wells JA, Aylward B, et al. Surgical removal of non-age-related subfoveal choroidal neovascular membranes. Eye 1998;12(Pt 5):775-80.
9. Sachdev N, Vishwanathan K, Gupta V, et al. Intravitreal bevacizumab (Avastin) in choroidal neovascular membrane in angioid streaks. Indian J Ophthalmol 2007;55(6):457-8.
10. Finger RP, Issa PC, Hendig D, et al. Monthly ranibizumab for choroidal neovascularisations secondary to angioid streaks in pseudoxanthoma elasticum: A one-year prospective study. Am J Ophthalmol 2011;152:695-703.
COMMENTS ARE WELCOME