Isotretinoin (13–cis-retinoic acid) is the first line treatment for moderate to severe nodulocystic or papulopustular acne [1,2]. Although it is a safe medication, it has several adverse side-effects, including ophthalmic manifestations, as shown in Table 1 [3]. These side-effects need to be recognised early, treated and / or referred to an ophthalmologist, to prevent significant ocular morbidity.

The exact mechanism of action of Isotretinoin is unclear, however, it is thought to induce apoptosis of certain cell types, including a cell type expressed in the Meibomian glands [6]. This gland is critical in maintaining the tear film by producing its external lipid layer, which prevents evaporation of the tear film [7]. There is contradictory research on the exact cause of tear film alterations. In vitro studies demonstrate exposure to 13–cis-retinoic acid inhibits cell proliferation, impacts gene expression and promotes inflammatory mediators, thus increasing the apoptosis on Meibomian glands [8]. However, studies also show patients with an impaired Schirmer test after Isotretinoin treatment, concluding that the retinoid effect is on tear film production itself [9]. In both circumstances, reducing the tear film volume increases the osmolarity of the tear fluid, which can damage the corneal epithelium [10]. These damaged cells undergo desquamation, leaving an erosion in the eye [11].
Case presentation
A 29-year-old woman awoke with a painful, red, watery left eye. The patient self-medicated with over the counter Hypromellose eye drops, every 30 minutes for one day, which resolved her symptoms. She did not seek any further medical attention. Two months later, the patient experienced the same symptoms, and presented to eye casualty. Slit-lamp examination with fluorescein staining, showed a left eye, 4mmx4mm corneal erosion. History noted the patient was taking Roaccutane (brand name of Isotretinoin) 80mg once daily, for four months. She was advised to use a hot compress every day, prescribed Hypromellose eye drops, VitA-POS eye ointment, and had follow-up in four weeks.
Within these four weeks, the patient had a further two episodes of waking overnight with left eye pain which resolved, on average, in 10 minutes. In the follow-up clinic, slit-lamp examination measured the erosion at 2.5mmx2.0mm with no infiltrate on the left cornea anteriorly, no anterior chamber reaction nor corneal oedema. The patient was advised to continue with regular Hypromellose and VitA-POS and in addition, Chloramphenicol eye drops, three times daily, for three days. Anterior stromal puncture and phototherapeutic keratectomy with excimer laser were discussed as treatment options, if symptoms persisted.

Figure 1: Papulopustular acne on patient’s face before (left) Isotretinoin treatment
and after (right) five months of Isotretinoin.
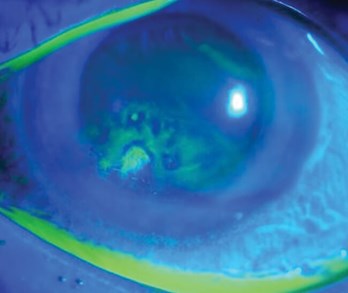
Figure 2: Fluorescein staining showing abnormal uptake suggestive of recurrent corneal erosion [16].
The patient was followed up within eight weeks, in which time, she had had a further six episodes of being unable to open left eye with ease and ocular pain. At follow-up, there was no change to visual acuity, but examination noted liner haze with punctate erosions in the left cornea. Considering the patient had ongoing significant meibomian gland dysfunction (MGD), Lymecycline was trialled to regulate the gland. She was further advised to increase the regularity of Hypromellose eye drop and VitA-POS, and to use a tea tree-based face wash, lid wipes and Omega 3 supplements. Punctal plug was discussed as a treatment option if these symptoms persisted. The patient was followed up in six months. During this period, the patient had a further 14 episodes, the majority being overnight. She had stopped taking Lymecycline, as was experiencing unpleasant side-effects. At follow-up, examination noted no change to the punctate erosions in the left cornea and the patient was recommended a heated eye mask whilst continuing all previous treatments.
The patient was seen again in clinic in four months’ time. In these months, the frequency of episodes reduced, and on average, the patient was having one episode a month. In clinic, slit-lamp examination noted significant improvement in the ocular surface, with improvement in tear film break-up time, corneal staining and Meibomian gland function. The patient had recently started using night eye goggles with artificial tears, based on her own research, which she noted made a ‘huge improvement’ in her symptoms. The patient has had delayed follow-up secondary to the COVID-19 pandemic and will be seen in clinic in the next few months.
Discussion
This case report is one of few published on Isotretinoin causing recurrent corneal erosions, although it appears to be an increasingly documented adverse side-effect. This patient’s experience highlights the importance of education to dermatologists initiating Isotretinoin treatment. Dry eye disease (DED) requires early recognition and can be initially managed by dermatology. Interestingly, a dermatology clinic letter reads the patient had to reduce frequency of contact lens wear, three months into her Isotretinoin course, as she had gritty sensations in her eyes.
Unfortunately, there were no recommendations for the patient to be aware that Isotretinoin can cause DED, to avoid contact lens wear and supplement dry eyes with artificial tears, lid hygiene and lifestyle changes. One could argue, if the patient’s gritty eye symptom was acted on and treated immediately, or referred to ophthalmology to rule out pathology, the chronic recurrent nature of the left eye erosion could have been minimised.
In current literature, treatment for DED is based on lifestyle changes, topical lubricants for tear insufficiency and lid hygiene [12-14]. Regarding lifestyle, patients should avoid windy, dry, air-conditioned environments, as well as reduce use of electronic devices, to lessen ocular surface desiccation [12]. This patient’s employment involved 24 hour on-call shifts. She was meticulous in keeping a symptom diary, which frequently noted acute episodes during overnight on calls, where the patient would have had increased screen time. Artificial tears and lid hygiene are the cornerstone in managing all severity grades of DED [14,15]. This patient only regularly started using Hypromellose eye drops and advised on lid hygiene once seen by an ophthalmologist. These recommendations can be readily prescribed by the dermatologist for patients on Isotretinoin, with DED symptoms. If more severe and / or unresponsive to treatment, it is necessary to refer to an ophthalmologist as treatment can be more complex and require specific equipment.
Conclusion
There is limited literature to guide dermatologists on recognising and treating DED related to Isotretinoin. As seen in this case, when left untreated, MGD can lead to a recurrent corneal erosion, causing a significant impact on the patient’s quality of life and ocular health. This case study proves the need for dermatologists to recognise and treat simple Isotretinoin-related ocular manifestations, such that ocular morbidity is reduced. Ultimately, Isotretinoin is clinically effective for acne vulgaris, however, close attention needs to be given to its side-effects. If patients present with DED, the dermatologist should prescribe artificial tears, offer lifestyle advice and provide lid hygiene steps to reduce the chances of DED causing recurrent corneal erosions.
References
1. Vallerand IA, Lewinson RT, Farris MS, et al. Efficacy and adverse events of oral isotretinoin for acne: a systematic review. Br J Dermatol 2018;178:76‐85.
2. Ahmad HM. Analysis of clinical efficacy, side effects, and laboratory changes among patients with acne vulgaris receiving single versus twice daily dose of oral isotretinoin. Dermatol Ther 2015;28:151‐7.
3. Brzezinski P, Borowska K, Chiriac A, Smigielski J. Adverse effects of isotretinoin: a large, retrospective review. Dermatol Ther 2017;30:e12483.
4. Aslan Bayhan S, Bayhan HA, Colgecen E, Gurdal C. Effects of topical acne treatment on the ocular surface in patients with acne vulgaris. Cont Lens Anterior Eye 2016;39:431-4.
5. Demirok G, Topalak Y, Gunduz O, et al. The long‐term effect of oral isotretinoin therapy on macula ganglion cell complex thickness. Cutan Ocul Toxicol 2017;36:259‑62.
6. Melnik BC. Apoptosis may explain the pharmacological mode of action and adverse effects of Isotretinoin, including teratogenicity. Acta Derm Venereol 2017;97:173‐81.
7. Gipson IK. The ocular surface: the challenge to enable and protect vision: the Friedenwald lecture. Invest Ophthalmol Vis Sci 2007;48(4390):4391‐8.
8. Ding J, Kam WR, Dieckow J, Sullivan DA. The influence of 13‐cis retinoic acid on human meibomian gland epithelial cells. Invest Ophthalmol Vis Sci 2013;54:4341‐50.
9. de Queiroga IB, Antonio Vieira L, Barros Jde N, et al. Conjunctival impression cytology changes induced by oral isotretinoin. Cornea 2009;28:1009‐13.
10. Mathers WD, Shields WJ, Sachdev MS, et al. Meibomian gland morphology and tear osmolarity: changes with Accutane therapy. Cornea 1991;10:286‐90.
11. Geerling G, Lisch W, Finis D. Rezidivierende Hornhauterosion bei epithelialen Hornhautdystrophien [Recurrent Corneal Erosions in Epithelial Corneal Dystrophies]. Klin Monbl Augenheilkd 2018;235(6):697-701.
12. Clayton JA. Dry eye. N Engl J Med 2018;378:2212‐23.
13. Lee YB, Koh JW, Hyon JY, et al. Sleep deprivation reduces tear secretion and impairs the tear film. Invest Ophthalmol Vis Sci 2014;55:3525‐31.
14. Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch Arztebl Int 2015;112(5):71-82.
15. Ngo W, Srinivasan S, Houtman D, Jones L. The relief of dry eye signs and symptoms using a combination of lubricants, lid hygiene and ocular nutraceuticals. J Optom 2017;10(1):26-33.
16. Dua HS. Resurfacing the ocular surface. Eye News 2016;22(6):12-8.
COMMENTS ARE WELCOME





