Keratoconus is an ectatic condition of the cornea characterised by progressive conical distortion with irregular astigmatism, myopia and apical protrusion. Most cases progress slowly resulting in varying degrees of myopic astigmatism. Management of keratoconus includes spectacles, soft contact lenses, a range of rigid gas permeable (RGP) contact lenses, hybrid contact lenses, piggyback systems, corneal collagen cross-linking (CXL), INTACS, phakic lens implants, and ultimately keratoplasty [1].
Fick first described the use of contact lenses to manage keratoconus in 1888. Despite the plethora of surgical options mentioned above, contact lenses remain one of the most successful options for the visual rehabilitation of mild to moderate cases and not only advanced cases [2]. It has been previously hypothesised but not proven that a rigid contact lens will delay progression of keratoconus by decreasing corneal scarring in sub-Bowman’s stroma [1,2].
Early forms of keratoconus can be successfully treated with soft contact lenses [1]. However, the gold standard treatment is with rigid contact lenses. A rigid lens will form a smooth refracting surface, with the liquid tear lens neutralising corneal surface irregularities. The main objective is to provide the best possible visual acuity, with a final fit that creates minimal interference to the corneal physiology. It is vital that the cornea continues to function well, without disturbing the epithelium.
Figure 1: Good alignment.

Figure 2: Steep fitting.

Figure 3: A flat fitting RGP – significant lens touch on the central cornea.
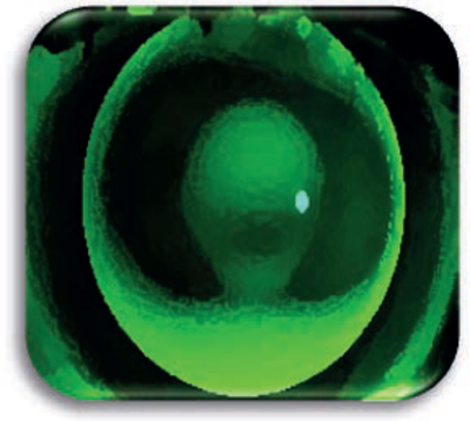
Figure 4: Three-point fit; minimal central and peripheral touch.
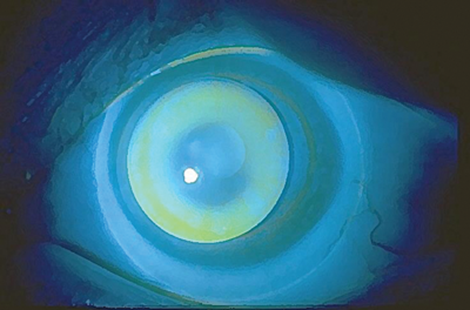
Figure 5: Piggyback fit.
Lens types
When considering the best lens choice in fitting a keratoconic patient, the shape, size of cone and location of the cone apex should be evaluated by careful slit-lamp examination, topography and tomography. The health of the entire ocular surface should also be carefully assessed.
Rigid gas permeable lenses (RGP lenses) designs may be spherical, aspherical or a combination of both. They are available in several different materials with varying oxygen permeability (Dk) values. In some cases of non-tolerance a ‘piggyback’ system may be adopted whereby a RGP lens is fitted over an underlying soft contact lens providing stability and comfort [3,4].
Hybrid contact lenses comprise of a soft peripheral portion and a high-Dk RGP centre. The diameter of the rigid central portion is 8.4mm and the total diameter of the lens is 14.5mm. The lens tends to remain stable on the eye of a patient with keratoconus, without decentering on horizontal or vertical eye movement, since the soft skirt provides stability by positioning the optics of the lens over the pupil [1,4].
Rose-K and Nissel K2 contact lenses consist of complex geometric designs manufactured on computerised lathes. The lenses can be fitted to most keratoconic patients, early or advanced, including asymmetric corneas. These lenses are delivered with aberration-control optics to provide best possible visual acuity at different lighting levels. They utilise gas permeable materials to optimise Dk values. When fitting such lenses one would aim for a minimal apical touch and a good peripheral fit [5].
Scleral lenses vault the cornea and extend onto the sclera. These lenses act by trapping a reservoir of fluid, hydrating the cornea and correcting irregular astigmatism by neutralising corneal irregularity. Scleral lenses are particularly useful for keratoconic patients who have poor lens handling, non-tolerance to conventional RGP lenses due to irritation of the lid margin by the lens edge and difficulty in centration of a corneal lens [1,6].
Factors to be considered when fitting contact lenses in keratoconic patients:
-
Optimising lens comfort – including piggyback / scleral lenses in selective cases
-
Lens movement – importance in promotion of tear exchange around the corneal cone
-
Positioning of the lens in relation to the pupil centre – often a compromise in keratoconus
-
Lenses should be adjusted dependant on disease progression
-
Increasing total lens diameter will improve comfort
-
A flat fitting will improve vision but risk increased corneal apical scarring
Lens fitting
The fitting of all rigid lenses in keratoconus requires keratometer readings, spectacle refraction, back vertex distance measurement, specification of the back optic zone radius and total diameter. A lens from a trial set is usually assessed or based on these measurements a trial contact lens can be ordered empirically. The back vertex power of the lens should be as close to the patient’s prescription. Corneal tomography and topography (e.g. Pentacam) are helpful in evaluating the shape, extent and location of the cone.
The trial lens fit requires assessment of both static and dynamic criteria.
- The lens should remain centred over the pupil in primary gaze and maintain reasonable centration on blinking.
- The lens should move approximately 1-1.5mm on blinking to allow metabolites and tear debris to be removed from underneath the lens. The movement should be smooth and unobstructed in the vertical plane.
- Fluorescein facilitates the assessment of lens alignment viewed using the slit-lamp or a Burton lamp. The ‘fluorescein pattern’ intensity allows confirmation of either a steep or flat fit of the lens. One should note the fluorescein intensity in the centre of the lens, mid peripheral and periphery (Figures 1-5).
- In fitting a RGP lens for a conical cornea, the ‘three-point-touch’ (Figure 4) is used to distribute the weight of the contact lens as evenly as possible between the cone and the peripheral cornea. With an apical contact area of 2-3mm aimed for [7].
- An over refraction should then be conducted to allow for the tear lens to be calculated. This measure gives further guidance on lens alignment. In a steep fitting lens (Figure 2) a positive tear lens results on over refraction, thus requiring less hypermetropic correction. This is often seen in apical clearance fitting, where the lens arches over the cone clearing the central cornea and resting paracentrally. Such a fit can be beneficial in reducing epithelial damage to the central cornea.
- A flat fitting lens (Figure 3) will result in a negative tear lens on over refraction. Here the lens is assumed to be fully on the cone and is characterised by a broad green band of lens clearance. This results in improved visual acuity due to the apical touch but may lead to increased apical changes and epithelial trauma [4].
- Ocular surface examination, including palpebral conjunctival and tear film assessment must be documented pre and post lens trial.
References
1. Romero-Jimenez M, Santodomingo-Rubido J, Wilffsohn JS. Keratoconus: a review. Contact Lens and Anterior Eye 2010;33:157-66.
2. Fick AE. A contact-lens.1888 (translation) Arch Ophthalmol 1988;106:1373-7.
3. Burns DM, Johnston FM, Frazer DG, et al. Keratoconus: an analysis of corneal asymmetry. Br J Ophthalmol 2004;88(10):1252-5.
4. Gasson A, Morris JA: The Contact Lens Manual: a practical guide to fitting. Oxford: Butterworth-Heinemann; 2003.
5. RoseK XL™ Semi-scleral Contact Lens Brochure. July 2012.
6. van der Worp E, Bornman D, Lopes Ferreira D, et al. Modern scleral contact lenses: a review. Contact Lens and Anterior Eye 2014;37;240-50.
7. Tomlinson M. The soft approach to RGPs. Bausch and Lomb Academy of Vision Care. August 2013:48-50.
Declaration of Competing Interests: None declared.
COMMENTS ARE WELCOME








