Optic neuritis is a relatively common presentation to ophthalmologists in the acute setting. The vast majority are cases of ‘typical’ optic neuritis (ON) but a smaller group of conditions, so-called, ‘atypical’ optic neuritides require a different work-up and management strategy. Selection of the correct management paradigm can significantly affect visual outcomes in some cases. The objective of this article is to help you make the clinical distinctions between typical and atypical optic neuritis.
What is optic neuritis?
An inflammation of the optic nerve characterised by swelling of the optic nerve (but not always), reduction of vision, and usually, marked reduction of colour vision.
What is typical optic neuritis?
Typical optic neuritis is a clinical synonym for idiopathic demyelinating optic neuropathy whether it is a clinically isolated syndrome (CIS) or one of multiple foci of demyelination in multiple sclerosis (MS). About 20% of patients with MS present with optic neuritis and 50% of MS patients suffer with optic neuritis during the course of their disease. About 50% of patients with CIS develop MS [1,2].
What is atypical optic neuritis?
Atypical optic neuritis is a heterogeneous collection of disorders whose presenting features suggest inflammation of the optic nerve. The inflammation may be triggered by an inflammatory or immune-related disease such as neurosarcoidosis, neuromyelitis optica or by a different process such as infection (e.g. syphilis).
What if we cannot find inflammation?
A diagnosis of atypical optic neuritis can be proven to belong to non-inflammatory diagnosis such as lymphoproliferative disease, vasculopathy or toxicity. If no inflammation is found on the basis of history and investigations, it is appropriate to classify an optic nerve pathology simply as an optic neuropathy.
Making the diagnosis and immediate management of typical and atypical optic neuritides
Clinical history
Take a detailed past medical history. This includes demographics (age and ethnicity), professional activity, habits, current or recent events (pregnancy, delivery), recent vaccinations or infections; periods of remission, and co-morbidities; concurrent or recent treatments (e.g. bone marrow transplant, new biological agents such as monoclonals) (Table 1).

Ask questions about the course of optic nerve dysfunction or neurological symptoms and the course of the recovery – both current and in the past. Specific questions, which should always be asked, include presence of diplopia, paraesthesia, vertigo, slurring of speech, weakness of one or more limbs, a history of ‘clumsiness’ e.g. dropping things frequently, bladder or bowel incontinence or lack of awareness of a full bladder, Uhtoff’s phenomenon (reduction of vision or deterioration of symptoms of demyelination elsewhere in the central nervous system (CNS)) when body temperature increases.
Clinical assessment
Visual acuity, colour vision measurement, pupil reflexes, field testing, cranial nerve examination and an eye examination are standard examinations. Involve neurologists early for new presentations to ensure a complete neurological assessment.
Although OCT of the retinal nerve fibre layer is often used in assessing the optic nerve, there is currently no evidence to support its value in distinguishing typical from atypical optic neuritis.
Diagnosis
In cases of atypical optic neuritis, a definitive diagnosis may not be achieved immediately after initial investigations but these results may guide further investigations. However, in a small group of patients, a conclusive diagnosis may prove elusive, especially if the disease is isolated to the optic nerve.
Table 3 contains four main subgroups of causes of atypical ON and the conditions listed are just some of many that may cause atypical ON.
Acute treatment
Typical optic neuritis
Intravenous corticosteroids may result in faster recovery to normal vision but have no effect on long-term visual prognosis [3]. They are of no benefit where vision is better than 6/12.
It is not always easy to be certain about whether a mild / moderate first isolated visual deficit is going to progress after assessment, especially if patient is seen very early in the course of inflammation.
Should the ophthalmologist or neurologist discuss MS risk? Yes, we feel that many people can become aware of an association between MS and optic neuritis through internet searches. It is usually best to acknowledge the information that is public from the outset, and counsel people that the association is known and the long-term risk but also the higher probability that a CIS is an isolated event.
Atypical optic neuritis
Acute treatment of atypical ON is similar to typical ON, unless there is a clear reason not to treat with corticosteroid. Start with high dose corticosteroids either orally or intravenously, followed by a reducing dose oral steroid programme.
- For any type of optic neuritis
where patients are given steroid treatment, patients should be given
contact information should symptoms deteriorate / new symptoms appear, especially if sight worsens after the steroids have stopped. - Monitor visual acuity, colour vision and visual fields at follow-up visits.
A patient-centred approach: counselling for optic neuritis
Counselling patients with optic neuritis is very important. It can be terrifying to lose vision rapidly and some patients will already be very anxious if they incorrectly perceive that they now have multiple sclerosis. Where a diagnosis is unclear, the uncertainty about vision worsening or disease recurrence can cause worry and fear. Do spend some minutes listening to your patients’ concerns.
For typical optic neuritis, it is very important to discuss the natural history of their condition including the high probability that vision will usually recover well and to discuss the risks and benefits of steroid treatment. (Faster recovery to normal if vision worse than 6/12 but no long-term difference in visual prognosis compared with those not treated with intravenous steroids). Patients should also be counselled that there is a risk of developing MS in the future. Although it is not possible to predict this, demyelinating lesions on MRI brain increases the risk of developing MS to 72% and absence of lesions, reduces this risk to 25% [4].
- Provide all patients with written information for future visits, investigations and contact
details for prompt
assessment if needed. - Monitor visual acuity, and colour vision and field tests at follow-up visits.
Case vignettes that highlight relevant features of typical and atypical optic neuritis
Case 1
A 36-year-old female presents with two week history of declining vision in the right eye, preceded by discomfort around the eye on movement for about three days. Vision is reduced to 6/36 on the right, there is a marked relative afferent pupillary defect (RAPD) and the disc is moderately swollen without any other ocular abnormalities. Colour vision is reduced to two Ishihara plates and visual field testing reveals a central and superior scotoma. She elected not to have steroid treatment and within four weeks, vision had returned to 6/9 with a persistent colour deficit to 12 Ishihara plates.
There was no previous relevant history. There were no symptoms on systems review and no other neurological history.
Diagnosis: This is typical optic neuritis. The key features are pain on eye movement, visual loss over a week and spontaneous visual recovery without steroids
Case 2
A 30-year-old Caucasian presented with the first episode of unilateral, painless visual loss in one eye upon waking. Crohn’s disease was diagnosed 18 months ago on colonoscopy after a single episode of colitis. She was on no medication. She presented with gross swelling of the optic nerve head on the right and swelling of the left optic nerve head. Vision was 6/36 on the right and 6/9 on the left.
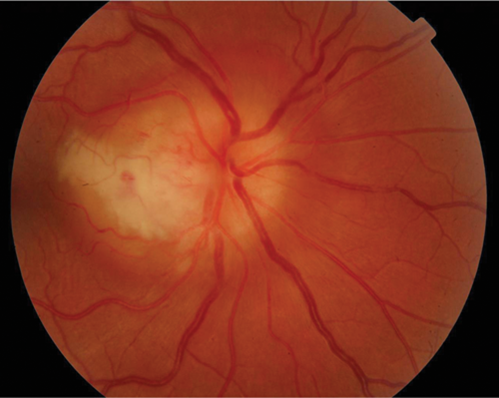
Figure 1 (top and above): Case 2 – right and left fundus.
There was a dense right RAPD, reduction in colour vision, a large, dense unilateral, nasal scotoma, and bilateral mild vitritis. MRI showed no white matter lesions. She was treated with high dose oral steroids with a residual dense nasal field defect and central visual acuity of 6/9. This is an atypical optic neuritis which may be associated with Crohn’s disease. Here the atypical features are the absence of pain, gross optic nerve head swelling and bilateral disease. The presence of intermediate uveitis is consistent with Crohn’s disease. The MRI findings support the likelihood that this pathological process was limited to optic nerve.
Case 3
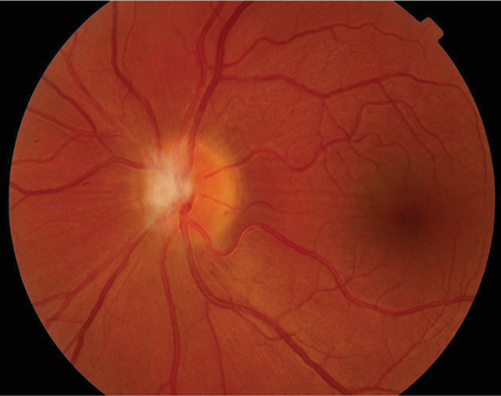
A 69-year-old Caucasian lady presented with painful, sequential, bilateral visual loss over six weeks. Vision was 6/60 on the right and CF left eye. Initially, the optic nerves were not swollen. There was a history of AChR antibody-positive myasthenia gravis. MRI showed high signal in both optic nerves and AQP4 ab was positive in the serum. She improved partially after high dose intravenous steroid for five days and is currently on long-term immunosuppression. This is an atypical optic neuritis where the key diagnostic features are bilateral, severe loss of vision over several weeks. The diagnosis of neuromyelitis optica is difficult to diagnose if it presents solely in the optic nerves and especially in the elderly. A past history of autoimmunity (myasthenia gravis) was critical in directing the investigation.
Figure 2: Case 3 – right (top) and left (bottom) optic nerves.
Case 4
A 21-year-old Asian man presented with bilateral, painful visual reduction over two weeks to 6/24 (right eye) and 6/60 (left eye) associated with reduced colour vision. Both optic nerve heads were swollen and associated with peripapillary haemorrhages and ‘macular star’ configuration of exudates indicating significant optic nerve oedema. Visual acuity returned rapidly on high dose intravenous steroid but deteriorated on stopping steroids after a tapering regime. Long-term immunosuppressive treatment was required to control inflammation. Investigations revealed optic nerve enhancement with contrast within the nerve sheaths and hilar adenopathy on CT Chest. He was diagnosed with systemic sarcoidosis after a bronchoscopy and exclusion of tuberculosis. This case is atypical due to the bilaterality, presence of apparent neuroretinitis as well as optic neuritis and recurrence of optic neuritis when steroids were reduced.


Figure 3 (top and above): Case 4 – right and left optic nerves.
Acknowledgements
All photos and case vignettes used in this article were reproduced with kind permission of the patients to whom they belong.
References
1. Balcer LJ. Clinical practice. Optic neuritis.
N Engl J Med 2006;354(12):1273-80.
2. Arnold AC. Evolving management of optic neuritis and multiple sclerosis. Am J Ophthalmol 2005;139(6):1101-8.
3. The Optic Neuritis Treatment Trial. A definitive answer and profound impact with unexpected results. Volpe, N Arch Ophthalmol 2008;126(7):996-9.
4. The Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final optic neuritis treatment trial follow-up. Arch Neurol 2008;65(6):727-32.
COMMENTS ARE WELCOME